Myelofibrosis is an uncommon type of bone marrow cancer that disrupts your body's normal production of blood cells.
Myelofibrosis causes extensive scarring in your bone marrow, leading to severe anemia that can cause weakness and fatigue.
What is the life expectancy of someone with myelofibrosis?
It does affect the life expectancy of the patients. The average survival is about 5 to 7 years. Unlike other myeloproliferative neoplasms, the name implies that these myeloid cells—they're the bone marrow cells—grow without control and overwhelm the bone marrow and blood
Is myelofibrosis a cancer?
Myelofibrosis is group of rare cancers of the bone marrow in which the marrow is replaced by scar tissue and is not able to make healthy blood cells. It is classified as a type of chronic leukemia and belongs to a group of blood disorders called myeloproliferative diseases.
Is there a cure for myelofibrosis?
A low-risk myelofibrosis may not require immediate treatment, while people with high-risk myelofibrosis may consider an aggressive treatment, such as bone marrow transplant. For intermediate-risk myelofibrosis, treatment is usually directed at managing symptoms.May
What causes myelofibrosis?
Primary myelofibrosis (MF) is a chronic blood cancer in which excessive scar tissue forms in the bone marrow and impairs its ability to produce normal blood cells. Researchers believe MF may be caused by abnormal blood stem cells in the bone marrow
Is myelofibrosis painful?
The result: achy or tender bones and joint tenderness. Growths: Blood cells are supposed to form inside your bone marrow. But myelofibrosis might cause them to grow in other parts of your body, like your lungs, liver, spleen, and digestive tract. ... They cause sharp pain, swollen joints, and inflammation.
Can you survive myelofibrosis?
Survival. Myelofibrosis, similar to other malignancies, is a serious disease. Published estimates of median survival in primary myelofibrosis range from 2.25 to 11.25 years, depending on risk level.
What are the symptoms of myelofibrosis?
As disruption of normal blood cell production increases, signs and symptoms may include:
Feeling tired, weak or short of breath, usually because of anemia.
Pain or fullness below your ribs on the left side, due to an enlarged spleen.
Easy bruising.
Easy bleeding.
Excessive sweating during sleep (night sweats)
Fever.
Can myelofibrosis be inherited?
The disorder is generally not inherited because this type of mutation does not affect the reproductive cells (sperm and egg) only certain cells of the body (somatic). Although myelofibrosis can occur at any age, it typically develops after the age of 50 years.
Does bone marrow transplant cure myelofibrosis?
Allogeneic transplantation is the only known curative treatment for myelofibrosis. Several studies have shown survival rates of 40–60% after allogeneic stem cell transplantation (Table 2). The first transplants for myelofibrosis used myeloablative conditioning, usually total body radiation or busulfan-based treatment.
What are the symptoms of bone marrow problems?
Symptoms of bone marrow cancer
weakness and fatigue due to shortage of red blood cells (anemia)
bleeding and bruising due to low blood platelets (thrombocytopenia)
infections due to shortage of normal white blood cells (leukopenia)
extreme thirst.
frequent urination.
dehydration.
abdominal pain.
loss of appetite.
Will I die from MDS?
And they will die of MDS. So how do you die of MDS if you don't develop acute myeloid leukemia? You die of MDS because of the increasing profundity of the blood counts. They fall so low that we cannot keep up with transfusions and supportive care measures anymore, and eventually they succumb to infection or bleeding.
What causes itching in myelofibrosis?
Itching occurs as a result of the activity of cytokines (small proteins involved in cell signaling) associated with myeloproliferative neoplasms (MPNs) and because a certain type of cell called a mast cell may release substances called histamines, which cause itching.
How serious is essential thrombocythemia?
Older people with essential thrombocythemia are at risk of complications. ... The abnormal blood clotting of essential thrombocythemia can lead to a variety of potentially serious complications, including: Stroke. A clot that blocks blood flow to your brain can cause a stroke.
Can myelofibrosis metastasize?
Myelofibrosis may occur as a result of the spread of cancer (metastasis) to bone marrow from primary tumors. ... Myelofibrosis may occur as a secondary characteristic of another bone marrow disorder such as polycythemia vera, multiple myeloma, certain metabolic disorders, and/or chronic myeloid leukemia.
What does a bone marrow biopsy feel like?
The doctor makes a small incision, then inserts a hollow needle through the boneand into the bone marrow. Using a syringe attached to the needle, the doctor withdraws a sample of the liquid portion of the bone marrow. You may feel a brief sharp pain or stinging. The aspiration takes only a few minutes.
Who gets myelofibrosis?
How common is myelofibrosis? Myelofibrosis is a rare condition, with about 1.5 cases reported per 100,000 people each year in the United States. It occurs in both men and women. People of any age can have myelofibrosis, although it is more likely to be diagnosed in people over age 50.
Does jakafi prolong life?
Jakafi can help to relieve the signs and symptoms of myelofibrosis, such as enlargement of the spleen, night sweats, itching, and bone or muscle pain. ... Patients with primary myelofibrosis who are categorized with intermediate-2 or high IPSS risk have a median life expectancy of 4 years or less.
Why does the spleen enlarge?
An enlarged spleen can be caused by infections, cirrhosis and other liver diseases, blood diseases characterized by abnormal blood cells, problems with the lymph system, or other conditions. Other causes of an enlarged spleen include: Inflammatory diseases such as sarcoidosis, lupus, and rheumatoid arthritis.
What does pain from spleen feel like?
A common symptom of an enlarged spleen is a feeling of pain or discomfort in the upper left side of abdomen, where the spleen is located. You might also experience a feeling of fullness after only eating a small amount. This usually happens when the spleen becomes enlarged to the point that it presses on the stomach.
Can bone marrow cause pain?
Bone pain can occur in leukemia patients when the bone marrow expands from the accumulation of abnormal white blood cells and may manifest as a sharp pain or a dull pain, depending on the location. The long bones of the legs and arms are the most common location to experience this pain.
What is fibrosis of the bone marrow?
Bone marrow fibrosis (BMF) is characterized by the increased deposition of reticulin fibers and in some cases collagen fibers.
What does bone pain feel like?
Bone pain is extreme tenderness, aching, or other discomfort in one or more bones. It differs from muscle and joint pain because it's present whether you're moving or not. The pain is commonly linked to diseases that affect the normal function or structure of the bone.
How long can a person live with myelofibrosis?
The average survival is about 5 to 7 years. Unlike other myeloproliferative neoplasms, the name implies that these myeloid cells—they're the bone marrow cells—grow without control and overwhelm the bone marrow and blood.
How much does jakafi cost?
The cost for Jakafi oral tablet 5 mg is around $13,697 for a supply of 60 tablets, depending on the pharmacy you visit. Prices are for cash paying customers only and are not valid with insurance plans.
Is jakafi chemo?
Jakafi is the first and only medicine approved by the Food and Drug Administration (FDA) for the treatment of these patients. Jakafi is not chemotherapy. It is a targeted treatment that works to help keep the production of blood cells under control.
Can you drink alcohol while taking jakafi?
The most common side effects of Jakafi include dizziness and headache. These are not all the possible side effects of Jakafi. ... Do not drink grapefruit juice while taking Jakafi.
What foods heal the spleen?
Sesame, pumpkin or sunflower seeds, legumes, kidney beans, lightly cooked vegetables, small amounts of lean meats, figs, coconuts, grapes, cherries, dates, potatoes, sweet potatoes, brown rice, oats, rice, ginger, spring onions and pu'er tea are among the best foods for the organ
Can coughing rupture your spleen?
Rupture of the spleen secondary to trauma is a potentially life- threatening yet relatively common complication. ... Spontaneous splenic rupture has been reported after trivial insults such as vomiting and coughing.
xxxxxxxxxxxxxxxxxxxxxxx
What is Primary myelofibrosis?
Primary myelofibrosis (also called chronic idiopathic myelofibrosis, agnogenic myeloid metaplasia) is a disorder in which normal bone marrow tissue is gradually replaced with a fibrous scar-like material. Over time, this leads to progressive bone marrow failure.
Under normal conditions, the bone marrow provides a fine network of fibres on which the stem cells can divide and grow. Specialised cells in the bone marrow known as fibroblasts make these fibres.
In primary myelofibrosis, chemicals released by high numbers of platelets and abnormal megakaryocytes (platelet forming cells) over-stimulate the fibroblasts. This results in the overgrowth of thick coarse fibres in the bone marrow, which gradually replace normal bone marrow tissue. Over time this destroys the normal bone marrow environment, preventing the production of adequate numbers of red cells, white cells and platelets. This results in anaemia, low platelet counts and the production of blood cells in areas outside the bone marrow for example in the spleen and liver, which become enlarged as a result.
Primary myelofibrosis is a rare chronic disorder diagnosed in an estimated 1 per 100,000 population. It can occur at any age but is usually diagnosed later in life, between the ages of 60 and 70 years. The cause of primary myelofibrosis remains largely unknown. It can be classified as either JAK2 mutation positive (having the JAK2 mutation) or negative (not having the JAK2 mutation).
Long-term exposure to high levels of benzene or very high doses of ionising radiation may increase the risk of primary myelofibrosis in a small number of cases. Around one third of people with myelofibrosis have been previously diagnosed with polycythaemia (post-polycythaemic myelofibrosis) or essential thrombocythaemia (post-ET myelofibrosis).
Symptoms and complications of primary myelofibrosis
Around 20 per cent of people have no symptoms of primary myelofibrosis when they are first diagnosed and the disorder is picked up incidentally as a result of a routine blood test. For others, symptoms develop gradually over time. Symptoms of anaemia are common and include unexplained tiredness, weakness, shortness of breath and palpitations. Other nonspecific symptoms include fever, unintended weight loss, pruritus (generalised itching) and excess sweating, especially at night.
Virtually all patients with primary myelofibrosis have an enlarged spleen (splenomegaly) when they are first diagnosed. In around a third of cases the spleen is very enlarged. Common symptoms include feelings of discomfort, pain or fullness in the upper left-side of the abdomen. An enlarged spleen may also cause pressure on your stomach causing a feeling of fullness, indigestion and a loss of appetite. Abdominal discomfort can also result from an enlarged liver (hepatomegaly), which occurs in around two-thirds of cases.
Other less common symptoms include bone and joint pain, and bleeding problems.
How is myelofibrosis diagnosed?
Primary myelofibrosis is diagnosed using a combination of a physical examination showing the presence of an enlarged spleen, blood tests and a bone marrow examination. Primary myelofibrosis is only diagnosed when other causes of marrow fibrosis (including leukaemia, lymphoma, other types of cancer that have spread to the bone marrow) have been ruled out.
Full blood count
People with primary myelofibrosis commonly present with varying degrees of anaemia. When examined under the microscope the red cells are often described as being ‘teardrop-shaped’. Higher than normal numbers of white cells and platelets may be found in the early stages of this disorder, but low white cell and platelet counts are common in more advanced disease.
Bone marrow examination
It is frequently impossible to obtain any samples of bone marrow fluid using a needle and syringe (bone marrow aspiration) due to marrow fibrosis. This is known as a ‘dry tap’. The bone marrow trephine biopsy typically shows abnormal fibrosis of the marrow cavity.
Cytogenetic and molecular analysis of blood and bone marrow cells is also carried out to help confirm the diagnosis and may help with prognosis. A mutation in JAK2 is found in about 50% of people with primary myelofibrosis. It is unclear at present why some patients with mutations in JAK2 develop myelofibrosis and others don’t.
How is myelofibrosis treated?
Some people have no symptoms when they are first diagnosed with primary myelofibrosis and do not require treatment straight away, apart from regular check-ups with their doctor to carefully monitor their disease.
For others treatment is largely supportive and is aimed at preventing complications due to low blood counts and an enlarged spleen (splenomegaly). This involves making every effort to improve your quality of life, by relieving any symptoms of anaemia or an enlarged spleen, and preventing and treating any complications that might arise from your disease or its treatment. This may include periodic blood transfusions and taking antibiotics to prevent and treat any infections.
A chemotherapy drug such as hydroxyurea, or low-doses of a drug called thalidomide may be used to reduce an enlarged spleen. In some cases, the surgical removal of the spleen (splenectomy) may be considered, especially when your spleen has enlarged so much that it is causing severe symptoms. A splenectomy may also be considered if you have an increased need for blood transfusions. This sometimes happens because the spleen is destroying blood cells, particularly platelets, at a very fast rate. Small doses of radiation to the spleen can also be given to reduce its size. This usually provides temporary relief for about 3 to 6 months.
Some younger patients who have a suitably matched donor may be offered an allogeneic (donor) stem cell transplant. This is a medical procedure that offers the only chance of cure for patients with myelofibrosis. It involves the use of very high doses of chemotherapy, with or without radiotherapy, followed by infusion of blood stem cells, which have been donated by a suitably matched donor. Stem cell transplants carry significant risks and are only suitable for a small minority of younger patients (usually under 60 years of age).
JAK2 inhibitors
JAK2 inhibitors work by blocking the activity of the JAK2 protein, which may lead to a reduction in splenomegaly and decreased symptoms. They also work in patients with myelofibrosis without the JAK2 mutation. Side effects may include worsening anaemia or a low platelet count.
Ruxolitinib is the only JAK2 inhibitor currently licenced for use in Australia. A number of JAK2 inhibitors may be available in clinical trials or may become available in the near future.
Prognosis
Primary myelofibrosis is generally regarded as an incurable disease but with treatment many people can remain comfortable and symptom-free for some time.
The natural course of the disease can vary considerably between individuals. In some people their disease remains stable for long periods and they are free to live a normal life with minimal interruptions from their disease or its treatment. For others, myelofibrosis progresses more quickly and people require treatment to help relieve symptoms of their disease. Transformation to a type of leukaemia called acute myeloid leukaemia occurs in between 10 and 20 per cent of cases.
Your doctor is the best person to give you an accurate prognosis regarding your disease as he or she has all the necessary information to make this assessment.Last updated on June 19th, 2019
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.
xxxxxxxxxxxxxxx
JAKAVI SIDE EFFECTS
Ruxolitinib
(rux oh LI ti nib)
Trade name: Jakafi™
Ruxolitinib is the generic for the trade drug Jakafi™. In some cases, health care professionals may use the trade name Jakafi™ when referring to the generic drug name ruxolitinib.
Drug type: Ruxolitinib is a targeted therapy. It is an oral receptor tyrosine kinase inhibitor - (For more detail, see "How this drug works," below.)
What Ruxolitinib Is Used For:
For the treatment of intermediate and high risk myelofibrosis.
For the treatment of acute graft-versus-host (GVHD) not responsive steroids, in adults and pediatric patients 12 years of older.
Note: If a drug has been approved for one use, physicians may elect to use this same drug for other problems if they believe it may be helpful.
How Ruxolitinib Is Given:
Ruxolitinib is a pill, taken by mouth, with or without food.
Take ruxolitinib exactly as prescribed, even if you are feeling better.
Swallow ruxolitinib tablets whole. Do not chew, crush or break.
Those who have feeding tubes may also use the tablet. Mix each tablet with 40 mL of water. Stir for 10 minutes. Give within 6 hours of mixing. Flush the feeding tube with water before and after this drug is given.
Do not change your dose or stop ruxolitinib unless your health care provider tells you to.
If a dose is missed, return to the usual dosing schedule. Do not take an additional dose.
Do not take extra doses of ruxolitinib. Call your health care provider right away if you take too much.
Avoid grapefruit, grapefruit juice, and supplements that contain grapefruit extract while taking ruxolitinib. Grapefruit products may increase the amount of ruxolitinib.
The amount of ruxolitinib that you will receive depends on many factors, your general health or other health problems, and the type of cancer or condition being treated.
Side Effects:
Important things to remember about the side effects of ruxolitinib:
Most people do not experience all of the side effects listed.
Side effects are often predictable in terms of their onset and duration.
There are many options to help minimize or prevent side effects.
There is no relationship between the presence or severity of side effects and the effectiveness of the medication.
The following side effects are common (occurring in greater than 30%) for patients taking ruxolitinib:
Anemia
Thrombocytopenia
These side effects are less common side effects (occurring in about 10-29%) of patients receiving ruxolitinib:
Increased liver enzymes
Diarrhea
Bruising
Swelling
Neutropenia
Dizziness
Increased cholesterol
Shortness of breath
Nasopharyngitis
Headache
Constipation
Nausea & Vomiting
Insomnia
Not all side effects are listed above. Some that are rare (occurring in less than 10% of patients) are not listed here. However, you should always inform your health care provider if you experience any unusual symptoms.
When to contact your doctor or health care provider:
Contact your health care provider immediately, day or night, if you should experience any of the following symptoms:
Fever of 100.4° F (38°C or higher, chills)
Signs of a very bad reaction (wheezing, chest tightness, fever, itching, bad cough, blue or grey skin color, seizures, or swelling or the face, lips, tongue or throat)
Always inform your health care provider if you experience any unusual symptoms.
The following symptoms require medical attention, but are not an emergency. Contact your health care provider within 24 hours of noticing any of the following:
Diarrhea (4-6 episodes in a 24-hour period)
Nausea (interferes with ability to eat and unrelieved with prescribed medication)
Vomiting (vomiting more than 4-5 times in a 24 hour period)
Unable to eat or drink for 24 hours or have signs of dehydration: tiredness, thirst, dry mouth, dark and decrease amount of urine, or dizziness
Skin or the whites of your eyes turn yellow
Urine turns dark or brown (tea color)
Decreased appetite
Pain on the right side of your stomach
Bleed or bruise more easily than normal
Signs of infection (very bad sore throat, ear or sinus pain, cough, more sputum or change in color of sputum, pain with passing urine, mouth sores, wound that will not heal or anal itching or pain)
Headache, back pain or joint pain
Skin changes (rash, acne, itching, blisters, peeling, redness or swelling)
Always inform your health care provider if you experience any unusual symptoms.
Precautions:
Ruxolitinib may interact with many types of medications. Before starting ruxolitinib treatment, make sure you tell your doctor about any other medications you are taking (including prescription, over-the-counter, vitamins, herbal remedies, etc.).
Do not receive any kind of immunization or vaccination without your doctor's approval while taking ruxolitinib.
Inform your health care professional if you are pregnant or may be pregnant prior to starting this treatment. Pregnancy category C (use in pregnancy only when benefit to the mother outweighs risk to the fetus).
For both men and women: Do not conceive a child (get pregnant) while taking ruxolitinib. Barrier methods of contraception, such as condoms, are recommended during treatment. Discuss with your doctor when you may safely become pregnant or conceive a child after therapy.
Do not breast feed while taking this medication.
Self-Care Tips:
Drink at least two to three quarts of fluid every 24 hours, unless you are instructed otherwise.
You may be at risk of infection so try to avoid crowds or people with colds, and report fever or any other signs of infection immediately to your healthcare provider.
Wash your hands often. Do not touch your eyes or the inside of your nose unless you have just washed your hands and have not touched anything else in the meantime.
Ask your doctor or nurse before scheduling dental appointments or procedures.
Use an electric razor to minimize bleeding.
Avoid contact sports or activities that could cause injury.
If you should experience nausea, take anti-nausea medications as prescribed by your doctor, and eat small frequent meals. Sucking on lozenges and chewing gum may also help.
Avoid sun exposure. Wear SPF 15 (or higher) sun block and protective clothing.
In general, drinking alcoholic beverages should be kept to a minimum or avoided completely. You should discuss this with your doctor.
Get plenty of rest.
Maintain good nutrition.
If you experience symptoms or side effects, be sure to discuss them with your health care team. They can prescribe medications and/or offer other suggestions that are effective in managing such problems.
Monitoring and Testing:
You will be checked regularly by your health care professional while you are taking ruxolitinib. Testing may include blood work that checks blood counts and liver functions.
How Ruxolitinib Works:
Targeted therapy is the result of about 100 years of research dedicated to understanding the differences between cancer cells and normal cells. To date, cancer treatment has focused primarily on killing rapidly dividing cells because one feature of cancer cells is that they divide rapidly. Unfortunately, some of our normal cells divide rapidly too, causing multiple side effects.
Targeted therapy is about identifying other features of cancer cells. Scientists look for specific differences in the cancer cells and the normal cells. This information is used to create a targeted therapy to attack the cancer cells without damaging the normal cells, thus leading to fewer side effects. Each type of targeted therapy works a little bit differently but all interfere with the ability of the cancer cell to grow, divide, repair and/or communicate with other cells.
There are different types of targeted therapies, defined in three broad categories. Some targeted therapies focus on the internal components and function of the cancer cell. The targeted therapies use small molecules that can get into the cell and disrupt the function of the cells, causing them to die. There are several types of targeted therapy that focus on the inner parts of the cells. Other targeted therapies target receptors that are on the outside of the cell. Therapies that target receptors are also known as monoclonal antibodies. Antiangiogenesis inhibitors target the blood vessels that supply oxygen to the cells, ultimately causing the cells to starve.
Ruxolitinib is a targeted therapy that targets and binds to the tyrosine kinase receptors and inhibits Janus Associated Kinases (JAK1 and JAK2) which mediate the signaling of a number of cytokines and growth factors that are important for hematopoiesis and immune function. By binding to these receptors, ruxolitinib blocks important pathways that promote cell division. Myelofibrosis (MF) is a myeloproliferative neoplasm (MPN) known to be associated with dysregulated JAK1 and JAK2 signaling. Patients with MF who either carry the JAK2 V617 mutation or does not have the JAK2 V617F mutation may both respond to ruxolitinib.
Research continues to identify which cancers may be best treated with targeted therapies and to identify additional targets for more types of cancer.
Note: We strongly encourage you to talk with your health care professional about your specific medical condition and treatments. The information contained in this website is meant to be helpful and educational, but is not a substitute for medical advice.





























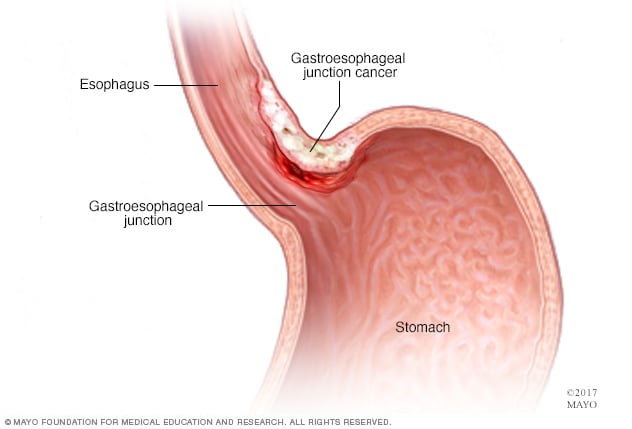
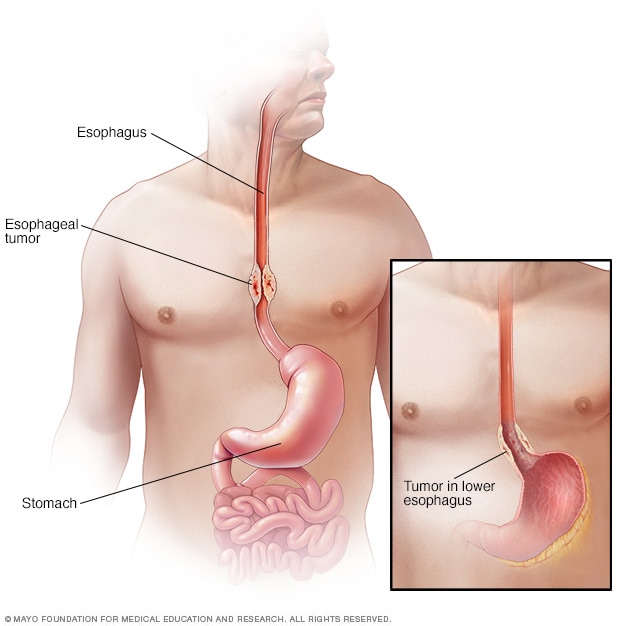
 EsophagusOpen pop-up dialog box
EsophagusOpen pop-up dialog box