HEALTH TID BITS BY RAM
Disclaimer: I am a Senior Citizen with multiple ailments and I have collated articles I have come across over time in this Blog to assist family and friends and Public in general. Having said that These are merely articles published by others and as such I don't take legal responsibility for any of the Contents. It is just for your Reading Pleasure and you decided whether it is Good or Not. Cheers
Search This Blog
Saturday, March 19, 2022
PHLEGM
PHLEGM
Phlegm (pronounced FLEM) is the secretions found in the throat including saliva, nasal secretions and sometimes acid secretions from the stomach. Phlegm becomes problematic if it interrupts voice production, breathing or swallowing. Too much phlegm may cause a “wet” or “gurgly” voice, or even difficulty swallowing. Increased amount of phlegm may cause one to clear his or her throat out often and repeatedly. Phlegm may also be a reason that individuals wake up at night. Phlegm normally thin in nature; however when it becomes thick it becomes difficult to tolerate. When there is not enough phlegm present that may become problematic as well.
Phlegm is mostly saliva, which is made by the salivary glands. There are four major salivary glands – two parotid glands located in front of the ears, and two submandibular glands located below the mandible or jaw bone. These four glands produce the majority of saliva. Sublingual glands, located below the tongue and minor salivary glands located throughout the mouth, throat and even the nose provide small contributions to the amount of saliva.
There are disorders where patients may complain of decreased secretions such as Sjogren’s syndrome. This is an autoimmune process in which individuals have dry eyes and dry mouth. Medications may also cause patients to complain of dry mouth as well. Finally, radiation used to treat head and neck cancer may cause salivary glands to produce less saliva that is often thick in quality.
Nasal secretions also contribute to phlegm. These secretions originate from the mucosa, or internal lining of the nose. For patients with allergic symptoms increased nasal secretions may drain into the throat, causing “too much phlegm”.
Acid reflux from the stomach also may contribute to phlegm. Acidic contents from the stomach may reflux, or travel backwards into the esophagus and throat. Acid from the stomach may be very irritating to individuals, causing problems of difficulty swallowing, cough, and even burning sensations in the throat.
Control of phlegm can be challenging because, as listed above, there are many contributions. Stepwise approaches considering these causes of phlegm may be necessary.
Sunday, February 20, 2022
Excess Mucus In The Throat.
Excess Mucus In The Throat – Causes And What Works Best
Though you may not be aware of it, the glands in your throat produce lots of mucus every day. Mucus, also known as phlegm, is essential for keeping your respiratory tract moist and healthy, and wards off infection. Excess mucus, however, can be unpleasant and bothersome and can cause a number of issues, including swallowing problems. Let’s take a look at what causes a build-up of mucus and some of the remedies that work best.
What Causes Excess Mucus In The Throat?
The stomach, nose, sinuses, and throat can all produce mucus, so getting a good diagnosis requires a medical examination. Possible causes of excess mucus can be food allergies, an acid reflux from the stomach, or an infection. The consistency of mucus in the throat also varies depending on what is going on in your body.

Common causes of too much mucus in the throat include a cold or flu, acute bronchitis, sinusitis or pneumonia. When mucus runs from the back of the nose down the throat after a meal, this could indicate an allergy. Causes can be mild, chronic, or severe (the onset of congestive heart failure), so be sure to seek medical advice.
Symptoms of mucus overproduction
Symptoms of excess mucus are coughing up phlegm, shortness of breath, or congestion in the throat. If the cause of mucus in the throat is a bacterial, viral, or fungal infection, symptoms may be different. They may include fever, itchy eyes, a runny nose, headache, and difficulty breathing. Frequent throat-clearing may be a symptom of stomach problems, as mucus formation is a protective mechanism against acidity.
What foods help excess mucus?
Some food and drinks tend to lead to a build-up mucus, while others relieve it. Things that help include broccoli, berries, oranges and greens, fatty fish like trout, and olive oil. Cayenne pepper, ginger, lemon, and herbal teas are also beneficial. Things that can aggravate mucus build-up include milk, soy, cheese, yoghurt, caffeine, processed meat, and alcohol.
Further tips and remedies
Many people with excess mucus find that sleeping with their head raised on an extra pillow helps. This is because elevating the head and shoulders in this way relieves congested nasal passages. Quit smoking and stay away from irritants and polluted air whenever possible. Blow your nose, inhale steam, gargle with salt and warm water, raise the humidity, diffuse essential oils, drink warm liquids. Remember dehydration is also bad, so make sure to drink a lot of water.
If your doctor diagnoses an allergy, allergy medications may help address the problem of excess mucus. Be aware of your swallowing and if you think something unusual is happening get medical advice. Another tip is not to eat a large meal before going to bed as this can cause indigestion and the production of more mucus.
Fairview Adult Day Care Center in Brooklyn NY pays close attention to the symptoms and causes of excess mucus as part of its comprehensive medical care regime. We provide education and guidance as to how to manage health issues in the elderly as well as people with neurological conditions.
Saturday, February 19, 2022
Salivary Gland Infections
Salivary Gland Infections
What’s a salivary gland infection?
A salivary gland infection occurs when a bacterial or viral infection affects your salivary gland or duct. The infection can result from reduced saliva flow, which can be due to a blockage or inflammation of your salivary duct. The condition is called sialadenitis.
Saliva aids digestion, breaks down food, and works to keep your mouth clean. It washes away bacteria and food particles. It also helps control the amount of good and bad bacteria in your mouth. Fewer bacteria and food particles are washed away when saliva doesn’t freely travel throughout your mouth. This may lead to infection.
You have three pairs of large (major) salivary glands. They’re located on each side of your face. Parotid glands, which are the largest, are inside each cheek. They sit above your jaw in front of your ears. When one or more of these glands is infected, it’s called parotitis.
Causes of salivary gland infection
A salivary gland infection is typically caused by a bacterial infection. Staphylococcus aureus is the most common cause of salivary gland infection. Others causes of salivary gland infection include:
Streptococcus viridans
Haemophilus influenzae
Streptococcus pyogenes
Escherichia coli
These infections result from reduced saliva production. This is often caused by the blockage or inflammation of the salivary gland duct. Viruses and other medical conditions can also reduce saliva production, including:
mumps, a contagious viral infection that’s common among children who haven’t been immunized
HIV
influenza A and parainfluenza types I and II
herpes
a salivary stone
a salivary duct blocked by mucus
a tumor
Sjogren’s syndrome, an autoimmune condition that causes dry mouth
sarcoidosis, a condition in which patches of inflammation occur throughout the body
dehydration
malnutrition
radiation cancer treatment of the head and neck
inadequate oral hygiene
Risk factors for infection
The following factors can make you more susceptible to a salivary gland infection:
being over age 65
having inadequate oral hygiene
not being immunized against mumps
The following chronic conditions also can increase your risk of developing an infection:
HIV
AIDS
Sjogren’s syndrome
diabetes
malnutrition
alcoholism
bulimia
xerostomia, or dry mouth syndrome
Symptoms of salivary gland infection
The following list of symptoms may indicate a salivary gland infection. You should consult your doctor for an accurate diagnosis. Symptoms of a salivary gland infection can mimic those of other conditions.
a constant abnormal or foul taste in your mouth inability to fully open your mouth
discomfort or pain when opening your mouth or eating
pus in your mouth
dry mouth
pain in your mouth
face pain
redness or swelling over your jaw in front of your ears, below your jaw, or on the bottom of your mouth
swelling of your face or neck
signs of infection, such as fever or chills
Contact your doctor immediately if you have a salivary gland infection and experience a high fever, trouble breathing or swallowing, or worsening symptoms. Your symptoms may require emergency treatment.
Potential complications
Salivary gland infection complications are uncommon. If a salivary gland infection is left untreated, pus can collect and form an abscess in the salivary gland.
A salivary gland infection caused by a benign tumor may cause an enlargement of the glands. Malignant (cancerous) tumors can grow quickly and cause loss of movement in the affected side of the face. This can impair part or all of the area.
In cases where parotitis happens again, severe swelling of the neck can destroy the affected glands.
You may also have complications if the initial bacterial infection spreads from the salivary gland to other parts of the body. This can include a bacterial skin infection called cellulitis or Ludwig’s angina, which is a form of cellulitis that occurs in the bottom of the mouth.
Diagnosis of salivary gland infection
Your doctor can diagnose a salivary gland infection with a visual exam. Pus or pain at the affected gland can indicate a bacterial infection.
If your doctor suspects a salivary gland infection, you may have additional testing to confirm the diagnosis and determine the underlying cause. The following imaging tests can be used to further analyze a salivary gland infection caused by an abscess, salivary stone, or tumor:
ultrasound
MRI scan
CT scan
Your doctor may also perform a biopsy of the affected salivary glands and ducts to test tissue or fluid for bacteria or viruses.
Treatment of salivary gland infection
Treatment depends on the severity of the infection, the underlying cause, and any additional symptoms you have, such as swelling or pain.
Antibiotics may be used to treat a bacterial infection, pus, or fever. A fine needle aspiration may be used to drain an abscess.
Home treatments include:
drinking 8 to 10 glasses of water daily with lemon to stimulate saliva and keep glands clear
massaging the affected gland
applying warm compresses to the affected gland
rinsing your mouth with warm salt water
sucking on sour lemons or sugar-free lemon candy to encourage saliva flow and reduce swelling
Most salivary gland infections don’t require surgery. However, it may be necessary in cases of chronic or recurring infections. Though uncommon, surgical treatment may involve removal of part or all of the parotid salivary gland or removal of the submandibular salivary gland.
Prevention
There’s no way to prevent most salivary gland infections. The best way to reduce your risk of developing an infection is to drink plenty of fluids and practice good oral hygiene. This includes brushing and flossing your teeth twice daily.
Saturday, February 12, 2022
GORD & Mucous in the Throat,
Somac - Long Term Use Side Effects
Fundic gland polyps warning: Long-term use (especially over one year) of pantoprazole can cause fundic gland polyps. These polyps are growths on the lining of your stomach that can become cancerous.
Important warnings
- nausea or vomiting.
- fever.
- rash.
- confusion.
- blood in your urine.
- bloating.
- elevated blood pressure.
Somac should not be taken for longer than 8 weeks. The dose and frequency of Somac that your doctor prescribes for you depends on your medical condition. Your doctor may change the dose as your condition changes.
Although PPIs have had an encouraging safety profile, recent studies regarding the long-term use of PPI medications have noted potential adverse effects, including risk of fractures, pneumonia, Clostridium difficile diarrhea, hypomagnesemia, vitamin B12 deficiency, chronic kidney disease, and dementia.
How long can you take pantoprazole 40 mg?
Adults—40 milligrams (mg) once a day for up to 8 weeks. Your doctor may want you to take pantoprazole for more than 8 weeks for certain conditions. Children 5 years of age and older weighing 40 kilograms (kg) or more—40 mg once a day for up to 8 weeks.
What is the safest drug for acid reflux?
Proton pump inhibitors are accepted as the most effective initial and maintenance treatment for GERD. Oral pantoprazole is a safe, well tolerated and effective initial and maintenance treatment for patients with non erosive GERD or erosive esophagitis.
Q. I developed a hoarse voice and annoying phlegm in my throat and was surprised to learn that the cause was acid reflux. I've never had heartburn, so I don't know how this could have happened. Can you explain what causes acid reflux?
A. It sounds as though you have a condition called laryngopharyngeal reflux (LPR). This occurs when stomach contents, including acid and enzymes, back up into the esophagus and injure the tissues of the larynx (voice box) and pharynx (throat). The cause is malfunctioning of the upper and lower esophageal sphincter muscles. These muscles are supposed to keep food moving in the right direction, from mouth to stomach. The lower esophageal sphincter prevents stomach acid from moving up the esophagus. When it malfunctions, stomach acid irritates the esophageal tissue immediately above the stomach, causing symptoms such as heartburn and chest pain with swallowing. This condition is called gastroesophageal reflux (GERD).
Laryngopharyngeal Reflux
In adults and children, irritating acidic juices may back up from the stomach into the esophagus (swallowing passage) and throat. This is frequently called gastroesophageal reflux disease or GERD. This condition may occur at any time, but it happens more often when you are laying down. A common anatomic condition known as a hiatal hernia predisposes people to acid reflux. The most commonly recognized symptom of acid reflux is “heartburn" due to irritation of the lining of the esophagus.
Most people do not know that acid reflux can also cause voice problems or symptoms in the pharynx (back of throat). This can happen to someone even if they are not aware of any heartburn and is sometimes called silent reflux, atypical reflux or laryngopharyngeal reflux.
The following information is intended to help you understand acid reflux and the steps you may take to reduce this problem. It is important to realize, however, that the healing of the irritated vocal folds, throat, or esophagus will take time, and you should not expect immediate results.
Symptoms in Adults
Symptoms of acid reflux may include:
- Hoarseness
- Excessive mucous or phlegm
- Throat clearing
- A sensation of a lump in the throat
- Sore throat
- Choking spells
- Wheezing
- A sense of post-nasal drip
Singers will often notice:
- Increased warm-up time
- Sluggish voice (particularly early in the day)
- A sense of a “coating" on the vocal folds
In a small percentage of people, more serious problems result, including:
- Pneumonia
- Ulcers or granulomas of the larynx
- Vocal fold scarring or a pouch (diverticulum) of the upper oesophagus
There is also a small chance of developing cancer in the esophagus or throat due to long-term acid reflux.
Thursday, February 3, 2022
Cystic Fibrosis
Request an Appointment
Patient Care & Health Information
Diseases & Conditions
Cystic fibrosis
Symptoms & causes
Diagnosis & treatment
Doctors & departments
Care at Mayo Clinic
Overview
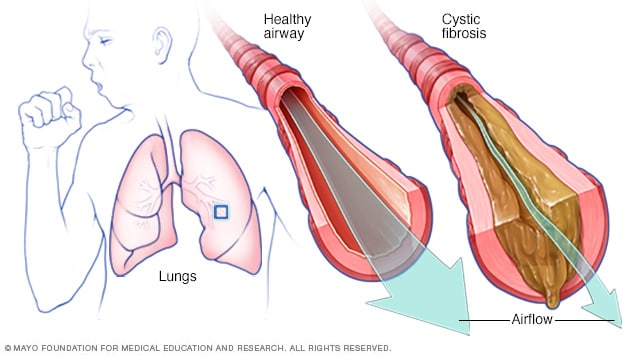 Cystic fibrosisOpen pop-up dialog box
Cystic fibrosisOpen pop-up dialog boxCystic fibrosis (CF) is an inherited disorder that causes severe damage to the lungs, digestive system and other organs in the body.
Cystic fibrosis affects the cells that produce mucus, sweat and digestive juices. These secreted fluids are normally thin and slippery. But in people with CF, a defective gene causes the secretions to become sticky and thick. Instead of acting as lubricants, the secretions plug up tubes, ducts and passageways, especially in the lungs and pancreas.
Although cystic fibrosis is progressive and requires daily care, people with CF are usually able to attend school and work. They often have a better quality of life than people with CF had in previous decades. Improvements in screening and treatments mean that people with CF now may live into their mid- to late 30s or 40s, and some are living into their 50s.
Products & Services
Book: Mayo Clinic Family Health Book, 5th EditionShow more products from Mayo Clinic
Symptoms
In the U.S., because of newborn screening, cystic fibrosis can be diagnosed within the first month of life, before symptoms develop. But people born before newborn screening became available may not be diagnosed until the signs and symptoms of CF show up.
Cystic fibrosis signs and symptoms vary, depending on the severity of the disease. Even in the same person, symptoms may worsen or improve as time passes. Some people may not experience symptoms until their teenage years or adulthood. People who are not diagnosed until adulthood usually have milder disease and are more likely to have atypical symptoms, such as recurring bouts of an inflamed pancreas (pancreatitis), infertility and recurring pneumonia.
People with cystic fibrosis have a higher than normal level of salt in their sweat. Parents often can taste the salt when they kiss their children. Most of the other signs and symptoms of CF affect the respiratory system and digestive system.
Respiratory signs and symptoms
The thick and sticky mucus associated with cystic fibrosis clogs the tubes that carry air in and out of your lungs. This can cause signs and symptoms such as:
A persistent cough that produces thick mucus (sputum)
Wheezing
Exercise intolerance
Repeated lung infections
Inflamed nasal passages or a stuffy nose
Recurrent sinusitis
Digestive signs and symptoms
The thick mucus can also block tubes that carry digestive enzymes from your pancreas to your small intestine. Without these digestive enzymes, your intestines aren't able to completely absorb the nutrients in the food you eat. The result is often:
Foul-smelling, greasy stools
Poor weight gain and growth
Intestinal blockage, particularly in newborns (meconium ileus)
Chronic or severe constipation, which may include frequent straining while trying to pass stool, eventually causing part of the rectum to protrude outside the anus (rectal prolapse)
When to see a doctor
If you or your child has symptoms of cystic fibrosis — or if someone in your family has CF — talk with your doctor about testing for the disease. Consult a physician who is knowledgeable about CF.
Cystic fibrosis requires consistent, regular follow-up with your doctor, at least every three months. Contact you doctor if you experience new or worsening symptoms, such as more mucus than usual or a change in the mucus color, lack of energy, weight loss, or severe constipation.
Seek immediate medical care if you're coughing up blood, have chest pain or difficulty breathing, or have severe stomach pain and distention.
Request an Appointment at Mayo Clinic
Causes
In cystic fibrosis, a defect (mutation) in a gene — the cystic fibrosis transmembrane conductance regulator (CFTR) gene — changes a protein that regulates the movement of salt in and out of cells. The result is thick, sticky mucus in the respiratory, digestive and reproductive systems, as well as increased salt in sweat.
Many different defects can occur in the gene. The type of gene mutation is associated with the severity of the condition.
Children need to inherit one copy of the gene from each parent in order to have the disease. If children inherit only one copy, they won't develop cystic fibrosis. However, they will be carriers and could pass the gene to their own children.
Risk factors
Because cystic fibrosis is an inherited disorder, it runs in families, so family history is a risk factor. Although CF occurs in all races, it's most common in white people of Northern European ancestry.
Complications
Complications of cystic fibrosis can affect the respiratory, digestive and reproductive systems, as well as other organs.
Respiratory system complications
Damaged airways (bronchiectasis). Cystic fibrosis is one of the leading causes of bronchiectasis, a chronic lung condition with abnormal widening and scarring of the airways (bronchial tubes). This makes it harder to move air in and out of the lungs and clear mucus from the bronchial tubes.
Chronic infections. Thick mucus in the lungs and sinuses provides an ideal breeding ground for bacteria and fungi. People with cystic fibrosis may often have sinus infections, bronchitis or pneumonia. Infection with bacteria that is resistant to antibiotics and difficult to treat is common.
Growths in the nose (nasal polyps). Because the lining inside the nose is inflamed and swollen, it can develop soft, fleshy growths (polyps).
Coughing up blood (hemoptysis). Bronchiectasis can occur next to blood vessels in the lungs. The combination of airway damage and infection can result in coughing up blood. Often this is only a small amount of blood, but it can also be life-threatening.
Pneumothorax. In this condition, air leaks into the space that separates the lungs from the chest wall, and part or all of a lung collapses. This is more common in adults with cystic fibrosis. Pneumothorax can cause sudden chest pain and breathlessness. People often feel a bubbling sensation in the chest.
Respiratory failure. Over time, cystic fibrosis can damage lung tissue so badly that it no longer works. Lung function usually worsens gradually, and it eventually can become life-threatening. Respiratory failure is the most common cause of death.
Acute exacerbations. People with cystic fibrosis may experience worsening of their respiratory symptoms, such as coughing with more mucus and shortness of breath. This is called an acute exacerbation and requires treatment with antibiotics. Sometimes treatment can be provided at home, but hospitalization may be needed. Decreased energy and weight loss also are common during exacerbations.
Digestive system complications
Nutritional deficiencies. Thick mucus can block the tubes that carry digestive enzymes from your pancreas to your intestines. Without these enzymes, your body can't absorb protein, fats or fat-soluble vitamins, so you can't get enough nutrients. This can result in delayed growth, weight loss or inflammation of the pancreas.
Diabetes. The pancreas produces insulin, which your body needs to use sugar. Cystic fibrosis increases the risk of diabetes. About 20% of teenagers and 40% to 50% of adults with CF develop diabetes.
Liver disease. The tube that carries bile from your liver and gallbladder to your small intestine may become blocked and inflamed. This can lead to liver problems, such as jaundice, fatty liver disease and cirrhosis — and sometimes gallstones.
Intestinal obstruction. Intestinal blockage can happen to people with cystic fibrosis at all ages. Intussusception, a condition in which a segment of the intestine slides inside an adjacent section of the intestine like a collapsible telescope, also can occur.
Distal intestinal obstruction syndrome (DIOS). DIOS is partial or complete obstruction where the small intestine meets the large intestine. DIOS requires urgent treatment.
Reproductive system complications
Infertility in men. Almost all men with cystic fibrosis are infertile because the tube that connects the testes and prostate gland (vas deferens) is either blocked with mucus or missing entirely. Certain fertility treatments and surgical procedures sometimes make it possible for men with CF to become biological fathers.
Reduced fertility in women. Although women with cystic fibrosis may be less fertile than other women, it's possible for them to conceive and to have successful pregnancies. Still, pregnancy can worsen the signs and symptoms of CF, so be sure to discuss the possible risks with your doctor.
Other complications
Thinning of the bones (osteoporosis). People with cystic fibrosis are at higher risk of developing a dangerous thinning of bones. They may also experience joint pain, arthritis and muscle pain.
Electrolyte imbalances and dehydration. Because people with cystic fibrosis have saltier sweat, the balance of minerals in their blood may be upset. This makes them prone to dehydration, especially with exercise or in hot weather. Signs and symptoms include increased heart rate, fatigue, weakness and low blood pressure.
Mental health problems. Dealing with a chronic illness that has no cure may cause fear, depression and anxiety.
Prevention
If you or your partner has close relatives with cystic fibrosis, you both may choose to have genetic testing before having children. The test, which is performed in a lab on a sample of blood, can help determine your risk of having a child with CF.
If you're already pregnant and the genetic test shows that your baby may be at risk of cystic fibrosis, your doctor can conduct additional tests on your developing child.
Genetic testing isn't for everyone. Before you decide to be tested, you should talk to a genetic counselor about the psychological impact the test results might carry.
By Mayo Clinic Staff
Cystic fibrosis care at Mayo Clinic
Thursday, January 13, 2022
Factors Contributing to Increased Platelet Reactivity in People With Diabetes,
Factors Contributing to Increased Platelet Reactivity in People With Diabetes
People with diabetes, particularly those with type 2 diabetes, exhibit increased platelet reactivity. Hyperglycemia contributes to greater platelet reactivity through direct effects and by promoting glycation of platelet proteins.
Platelets from subjects with diabetes exhibit increased reactivity (i.e., increased propensity to activate in response to a stimulus) (1). This review highlights factors that contribute to increased platelet reactivity. Type 2 diabetes is more prevalent than type 1 diabetes and is associated with a substantially increased risk of macrovascular complications. Accordingly, this review focuses on platelet reactivity in subjects with type 2 diabetes. Key aspects of type 2 diabetes are insulin resistance, metabolic abnormalities including hyperglycemia, and systemic abnormalities including oxidative stress and inflammation. The influence of each of these abnormalities on platelet function is addressed.
Go to:
Metabolic abnormalities and platelet function
Induction of hyperglycemia and hyperinsulinemia in healthy subjects without diabetes increases platelet reactivity (2). Consistent with this observation, improved glycemic control has been associated with decreased platelet reactivity (3). Hyperglycemia can increase platelet reactivity by inducing nonenzymatic glycation of proteins on the surface of the platelet. Such glycation decreases membrane fluidity and increases the propensity of platelets to activate (4). Osmotic effect of glucose is a second mechanism by which hyperglycemia can increase platelet reactivity (5). We found that brief exposure of platelets in vitro to hyperglycemia or a similar concentration of mannitol increased their reactivity. Activation of protein kinase C is a third mechanism by which hyperglycemia can increase platelet reactivity (6). Protein kinase C is an essential mediator of platelet activation.
People with diabetes exhibit increased expression of the surface glycoproteins Ib and IIb/IIIa (7). These glycoproteins mediate platelet adhesion and adherence. Thus, greater expression would be anticipated to increase the functional activity, if not the reactivity, of platelets in subjects with diabetes. Expression of these adhesion proteins correlates with hyperglycemia reflected by A1C.
Although hyperglycemia is the sine qua non of diabetes, abnormalities of lipid metabolism are uniformly observed.
Go to:
Insulin resistance, insulin deficiency, and platelet function
Most people who are destined to develop type 2 diabetes exhibit insulin resistance and consequent hyperinsulinemia for 1–2 decades before manifesting diabetes. During this interval, hyperinsulinemia compensates for insulin resistance and fasting hyperglycemia is not evident. Obesity can induce and exacerbate insulin resistance. Apoptosis of pancreatic β-cells leads to a relative and ultimately absolute deficiency of insulin. Progressive insulin deficiency is seen after type 2 diabetes becomes manifest. Both insulin resistance and insulin deficiency can alter platelet reactivity.
Insulin antagonizes the effect of platelet agonists such as collagen, ADP, epinephrine, and platelet-activating factor (9). This antagonism is mediated by activation of an inhibitory G protein by insulin receptor substrate (IRS)-1 (10). Insulin resistance reflects impaired insulin signaling, predominantly mediated by IRS.
Obese subjects who are insulin resistant exhibit increased activation of platelets. Platelet activation identified by the measurement of a thromboxane metabolite in urine and the concentration of CD40 ligand in blood was increased in obese compared with lean women.
As mentioned previously, subjects with type 2 diabetes exhibit progressive deficiency of insulin as a consequence of pancreatic β-cell apoptosis. A consequence of pancreatic β-cell apoptosis is absolute deficiency of insulin. Accordingly, the relative deficiency of insulin imparted by insulin resistance is magnified by the superimposition of insulin deficiency. Platelet reactivity that is increased in obese subjects manifesting insulin resistance will be greater when type 2 diabetes is manifest and accompanied by absolute deficiency of insulin.
A recent study suggests that resistance to the effects of insulin is apparent in pathways independent of IRS in addition to those dependent on IRS (13). Consistent with this observation, platelets from subjects with insulin resistance show diminished sensitivity to the actions of NO and prostacyclin (14,15). NO and prostacyclin are produced by the intact endothelium and retard platelet activation by increasing intraplatelet concentrations of cyclic nucleotides, cyclic guanosine monophosphate, and cyclic adenosine monophosphate. Thus, resistance of the platelet to the effects of these agents promotes increased platelet reactivity. Accordingly, insulin resistance attenuates tonic antagonism of platelet activation and thereby increases platelet reactivity.
Go to:
Oxidative stress, inflammation, and platelet function
Diabetes is associated with systemic inflammation and oxidative stress that may contribute to increased platelet reactivity. Superoxide has been shown to increase platelet reactivity (16). One mechanism by which superoxide may increase platelet reactivity is by enhancing intraplatelet release of calcium after activation (17). In addition, superoxide limits the biologic activity of NO (18). Attenuating the effect of NO would be anticipated to increase platelet reactivity. Oxidative stress impairs endothelial function and reduces production of NO (19). Impaired endothelial function also decreases the production of prostacyclin (20). Accordingly, oxidative stress that accompanies diabetes promotes greater platelet reactivity through direct effects on platelets and by inducing endothelial dysfunction. Endothelial dysfunction increases platelet reactivity because of decreased production and effect of NO and decreased production of prostacyclin.
Thrombosis that entails platelet activation is intimately intertwined with inflammation. People with diabetes exhibit increased markers of both platelet activation and inflammation (21). In particular, cross-talk between platelets and leukocytes amplifies leukocyte activation both by platelet activation and by platelet reactivity (22). For example, the release of platelet-activating factor by leukocytes primes platelets for activation and increases the extent to which they activate in response to other agonists (23).
An additional mechanism by which inflammation can increase platelet reactivity is by increasing expression of proteins that participate in the activation of platelets. For example, subjects with diabetes exhibit increased expression of Fcγ receptor type IIa (FcγRIIa) and associated increased platelet activation in response to collagen (24). Inflammation appears to increase expression of FcγRIIa, and attenuation of inflammation decreases expression of FcγRIIa (25). Thus, inflammation that accompanies diabetes contributes to increased platelet reactivity that, in turn, contributes to greater inflammation.
Go to:
Summary
Diabetes is associated with increased platelet reactivity. Factors that contribute directly to greater platelet reactivity include metabolic abnormalities such as hyperglycemia and hyperlipidemia, both insulin resistance (relative insulin deficiency) and absolute insulin deficiency, as well as associated conditions such as oxidative stress, inflammation, and endothelial dysfunction. Although antiplatelet therapy is necessary to suppress increased platelet reactivity, control of hyperglycemia with regimens that decrease insulin resistance and prevent apoptosis of pancreatic β-cells should decrease platelet reactivity and enhance the efficacy of antiplatelet therapy by addressing root causes of increased reactivity.
Go to:
Acknowledgements
No potential conflicts of interest relevant to this article were reported.
Go to:
REFERENCES
1. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Ramírez C, Sabaté
Thursday, December 23, 2021
Gastrointestinal bleeding - Mayo Clinic
Gastrointestinal bleeding
Symptoms & causes
Diagnosis & treatment
Doctors & departments
Care at Mayo Clinic
Diagnosis
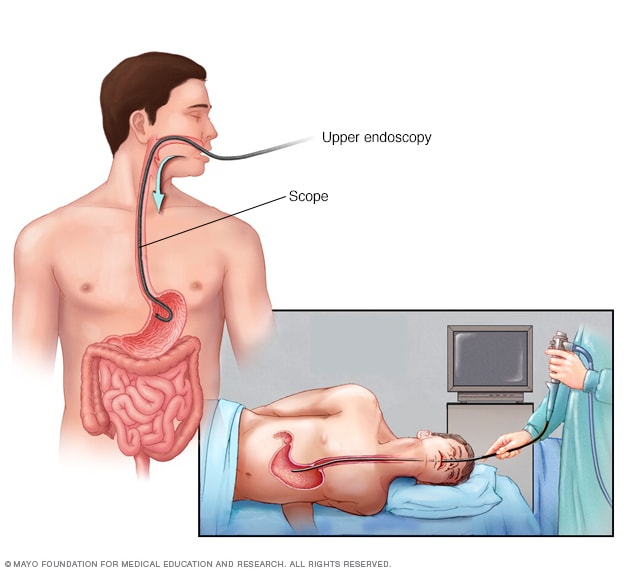 EndoscopyOpen pop-up dialog box
EndoscopyOpen pop-up dialog boxYour doctor will take a medical history, including a history of previous bleeding, conduct a physical exam and possibly order tests. Tests might include:
Blood tests. You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests.
Stool tests. Analyzing your stool can help determine the cause of occult bleeding.
Nasogastric lavage. A tube is passed through your nose into your stomach to remove your stomach contents. This might help determine the source of your bleed.
Upper endoscopy. This procedure uses a tiny camera on the end of a long tube, which is passed through your mouth to enable your doctor to examine your upper gastrointestinal tract.
Colonoscopy. This procedure uses a tiny camera on the end of a long tube, which is passed through your rectum to enable your doctor to examine your large intestine and rectum.
Capsule endoscopy. In this procedure, you swallow a vitamin-size capsule with a tiny camera inside. The capsule travels through your digestive tract taking thousands of pictures that are sent to a recorder you wear on a belt around your waist. This enables your doctor to see inside your small intestine.
Flexible sigmoidoscopy. A tube with a light and camera is placed in your rectum to look at your rectum and the last part of the large intestine that leads to your rectum (sigmoid colon).
Balloon-assisted enteroscopy. A specialized scope inspects parts of your small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test.
A contrast dye is injected into an artery, and a series of X-rays are taken to look for and treat bleeding vessels or other abnormalities.
Imaging tests. A variety of other imaging tests, such as an abdominal CT scan, might be used to find the source of the bleed.
If your GI bleeding is severe, and noninvasive tests can't find the source, you might need surgery so that doctors can view the entire small intestine. Fortunately, this is rare.
Care at Mayo Clinic
Sunday, November 14, 2021
Myelo Fibrosis,
By Mayar, Facty StaffUpdated:
Myelofibrosis is a type of cancer that affects bone marrow. Bone marrow is the part of the body that is responsible for forming new blood cells. You may think of bone marrow as a factory for making blood cells. In myelofibrosis fibrosis, a certain gene mutation causes the bone marrow to produce a lot of blood cells at some stage. Abnormal cells in the bone marrow start to produce certain substances called cytokines. One of these cytokines is called fibroblast growth factor, which replaces the tissue that forms blood cells by collagen fibrous tissue. This will decrease the bone marrow's ability to produce new blood cells, so the numbers of all types of blood cells will decrease which is called "pancytopenia."
1. The abdomen may feel Swollen
The abnormal blood cells may collect in the liver and spleen. Because there is a significant number of them and because they tend to grow rapidly, they can cause the liver and spleen to increase in size. That is why people affected by myelofibrosis will start to feel that their abdomen is swollen. They may also feel fullness or heaviness.

2. Fatigue
In myelofibrosis, the tissue that forms blood cells is replaced by collagen fibrous tissue. This will decrease the bone marrow's ability to produce new blood cells. Some of these affected cells are red blood cells. This is why the person who suffers from Myelofibrosis can develop anemia.
The decrease in the number of available red blood cells will cause many other symptoms as well. Fatigue is one of them because red blood cells are responsible for delivering oxygen to all of the cells in the body. When the numbers of red blood cells decrease, the different cells of the body will not be able to find an adequate amount of oxygen that it needs to produce energy. So, the person will feel tired and exhausted all the time.

3. Pale skin
This is also caused by the decreased numbers of red blood cells. The blood running through the vessels is what gives the skin its pinkish color, and the blood appears red in color because it contains red blood cells. Red blood cells are red because they contain red subunit called heme. Heme subunits are part of the hemoglobin protein of the red blood cells. It can help in binding Iron which, in turn, helps in binding oxygen. When there are less red blood cells, the blood will contain a lesser amount of that subunit. So, the skin will appear paler.

4. Dizziness and Shortness of breath
Because the number of red blood cells decreases, the cells in the brain do not get an adequate amount of oxygen they need for various function. This makes the person affected with Myelofibrosis feel dizzy and lightheaded. Many Patients may find it hard to focus, concentrate or perform challenging mental activities. They may also experience breathing difficulties in the form of shortness of breath. This shortness of breath becomes more obvious when the person tries to do some physical activity. It is also caused by a decreased number of red blood cells.

5. Infection
White blood cells are a crucial and vital part of the body's defense system. They help protect the body from many harmful organisms. In Myelofibrosis, the tissues responsible for producing white blood cells are replaced by fibrous tissue. This makes the bone marrow produce less White blood cells. That is why myelofibrosis patients have a low immunity and are more likely to get sick than normal people.

6. Bruising and easy bleeding
The fibrosis of parts of the bone marrow decreases its production of platelets as well. Platelets play a major role in forming clots and stopping the bleeding. The low number of platelets is scientifically termed "thrombocytopenia." It will lead to petechiae and bleeding from the gums, nose and under the skin. Petechiae are small red spots on the skin or mucous membrane resulting from bleeding of a small capillary vessel. Small petechiae can group together to form a larger purple or blue spot called ecchymoses. Myelofibrosis will also experience bleeding from minor trauma and an increase in the time needed so that the bleeding stops.

7. Bone pain
Some people with Myelofibrosis will experience some form of bone pain. It is a relatively common symptom. It occurs commonly in the long bone. Long bones are a type of bone present in the human body. The Femur, tibia, and fibula are examples of long bones. Pain in the joints, as well as inflammation in the joints, are also commonly associated with bone pain.

8. Weight loss
The people affected by myelofibrosis feel tired and exhausted all the time. This feeling is present even with no or minimal effort. As a direct result of their disease, they may start to lose their appetite and eat less or refuse to eat. This will may make them lose weight. The combination of fatigue, appetite loss, and weight loss will lead to a type of weakness that may progress to wasting of the body that is common in severe chronic disease. This is called cachexia, and it is also common in patients who have other types of cancers.

9. Gout and high uric acid levels
Myelofibrosis can increase the levels of uric acid in the blood. The cause of this high uric acid level is not yet clear. It is possible that myelofibrosis makes the body produce more uric acid or decreases the body's ability to remove it. High levels of uric acids are known as Gout. Some of the symptoms that indicate a person has developed gout include pain and swelling of the joint of the big toe, redness around the joint, and limitation of the movement of the joint.

10. Cutaneous myelofibrosis
Cutaneous myelofibrosis is a rare condition that usually happens in neonates who are exposed to an intrauterine infection; or those who are born with certain diseases like hereditary spherocytosis and twin transfusion syndrome. It affects the skin and leads to the formation of nodules in the dermis and the subcutaneous tissue of the skin.
10 Treatments for Bone Cancer
HomeConditionsCancer
By Charmaine, Facty
Bone cancer is a cancerous tumor of the bone. There are both benign (noncancerous) tumors and malignant (cancerous) bone tumors, but only the malignant tumors destroy healthy bone density tissue. Benign tumors also grow in the body but do not spread, or destroy any bone tissue and are not usually a threat to life. A malignant tumor is primary bone cancer and is less common than cancer that metastasizes (spreads) to the bones in other parts of the body. Of primary bone cancer, there are a few different kinds, including Osteosarcoma, Chondrosarcoma and Ewing Sarcoma. There are many roads to go down in regards to treatment, but it’s a matter of finding the right one for your specific kind of bone cancer.
1. Radiation
Radiation therapy, also known as Radiotherapy, is often used in those suffering from bone cancer as secondary cancer. It helps to control the pain and also helps prevent the development of new pain. You can have either External Beam Therapy, which is when a radiation beam is directed at the bone, from outside the body or, Internal Radiotherapy. With this, you have an injection of radiation liquid, which is injected directly into the affected area and lasts for a couple of days in your body. Radiotherapy will not cure cancer but, it will slow the cancer growth and give you a better quality of life.

2. Chemotherapy
Targeting cancer that begins in your bones, chemotherapy uses a combination of anti-cancer drugs injected into the bloodstream, to destroy the cancer cells. Although chemotherapy works very well for different types of cancer, you may treatments at various stages of cancer. Before or after surgery to reduce the risk of the cancer returning, and sometimes you may have it along with radiotherapy. A course of treatment is made up of between 6-14 cycles. One cycle is a dose of drugs over many days in a hospital, then a break of a couple of weeks. If the cancer is advanced, you may have a course of chemotherapy to prolong life by slowing cancer and relieving symptoms.

3. Targeted therapy
Targeted therapy in bone cancer is when drugs are used to stop the growth and spread of cancer. It does this by killing the cancer cells, preventing the cancer cells from multiplying. It is called ‘targeted’ because they use a mix of drugs specifically chosen with regard to the patient’s type of cancer and their DNA. These drugs can be taken orally with pills at home or intravenously at the hospital. Not all cancers can be treated in this method, and the schedule of drugs is different in each patient. Targeted therapy can also be used in conjunction with chemotherapy and radiation therapy or surgery.

4. Surgery
Surgery for bone cancer is an option when other treatments have not been successful, or when your health professional decides cancer needs to come out of your body as soon as possible. The type of surgery needed depends on the size of cancer and where it is. Surgery includes removing the bone affected, or removing a part of the bone affected and replacing it with a prosthetic piece. This surgery is usually only used when the cancer is not attached to any other tissues surrounding the bone. Surgery is also used in amputation. By removing the entire arm or leg that was infected by cancer.

5. Mifamurtide medication
For a particular bone cancer called osteosarcoma, which usually affects children and young adults, a medication called Mifamurtide can be administered in combination with chemotherapy. A course of Mifamurtide will begin after surgery, to help prevent cancer returning. This drug works by stimulating the immune system to produce particular specialized cells, which kill the cancer cells. Taken by infusion, a course of treatment can be two times a week for 12 weeks then once a week for another 24 weeks.

6. Massage therapy
Massage therapy is not a cure for bone cancer, but studies have found that massage helps the wellbeing of cancer sufferers. Massage is used as a natural way to help cope with cancer and cancer treatments. Massage can help by reducing symptoms like some pain and nausea, anger and stress, fatigue, anxiety, and depression. Massage is used to help cancer patients feel better. Cancer patients interested in using massage to reduce the stress of the disease will have to find a professional massage therapist that can work with those patients currently having treatment.

7. Diet
Naturally, proper nutrition and eating well is essential for anyone’s health. When you have bone cancer and need treatment, your eating habits will change dramatically, your appetite will go up and down and tolerance to various food swill change. Before treatment, it is crucial to eat well, so you are better equipped to handle the side effects of the drugs. You need strength and a boost in your immune system to handle the treatment better. Foods high in protein and calories are best. During your treatment will be the hardest as you most likely won’t feel like eating anything so choose well when you decide what to put in your body. After treatment, it’s best to stick to low-fat milk and dairy, high fiber foods and lots of fruits and vegetables.

8. Vitamins and supplements
When in cancer treatment you are putting your body through a great deal. Along with a nutritional diet, it is important to take some dietary supplements and vitamins to make sure your body is receiving all the good things you need to stay healthy. It’s recommended to take multivitamins containing A, C, E< and B complex; also important are magnesium, calcium selenium and zinc. A probiotic is good to take to maintain gastrointestinal health and boosting your immune system. Fish oil can help to decrease inflammation, and for bone support, it is imperative to take Vitamin D and Calcium Citrate.

9. Yoga
Studies have shown that yoga can help manage depression, anxiety, and fear. Most of these things are prevalent in cancer suffers. When practiced during cancer treatment, pain and fatigue caused by the treatment can be significantly improved. What you learn in yoga about breathing techniques, as well as strengthening the body’s core, have an effect on the outlook and pain tolerance of cancer patients. You can expand your range of motion, improve circulation and reduce muscle tension, all beneficial for those going through a medical cancer treatment. You don’t have to be a professional yogi to reap the benefits of some of the key exercises, practiced regularly.

10. Aloe vera
Aloe vera is one of the most powerful plants around. It contains massive healing qualities and is full of vitamins like B1m B2, B3, B5, B6, B12 Vitamin C, and choline, plus zinc, calcium, copper, magnesium, and manganese. It’s this concoction, which is beneficial for bones. Aloe is often used in cancer patients directly onto the skin of those having radiotherapy, lessening the reaction in the skin. There have also been studies to suggest aloe taken in liquid form while on a cycle of chemotherapy, helped shrink the size of cancer. There are some side effects to ingesting large amounts of aloe vera so please talk to your doctor for more information.

10 Signs Of Bone Cancer
HomeConditionsCancer
By Glenda Taylor
Reviewed By Brindusa Vanta, MDUpdated: Apr 27, 2020
Primary bone cancer is rare, making up around 0.2 percent of all cancers, according to the American Society of Clinical Oncology. Researchers say the onset could be linked to hereditary factors, but a specific cause is not known. The majority of bone tumors are noncancerous. In many cases, when cancer is found in the bone it is secondary -- the tumors spread or metastasized from somewhere else and are thus not categorized as bone cancer. Bone cancer, or cancer that has reached the bones, has a variety of symptoms.

2. Tingling, Numbness, or a Burning Sensation
When bone cancer affects the nerves inside the bone, individuals describe a tingling, numb, or burning sensation. Nerve pain can be difficult to describe to a physician because it is unlike the usual types of pain. Bone cancer disrupts the normal activity of bone cells, irritating the interior nerves, injuring the nerve fibers, and increasing nerve sensitivity. Oncologists say that once the tumors interact with the nerves inside the bone, the tumor size increases, worsening these symptoms.

3. Joint Stiffness and Swelling
Bone cancers often develop near or in a joint in the upper arms or legs. Not only does the area around the joint become tender, but the tumor also causes stiffness, which affects the range of motion. Swelling and redness then develop in the area where the pain first developed, usually several weeks later. The individual may notice a lump or mass near the area as well. A physician will check the area for swelling and tenderness and changes in the surrounding skin.

4. Weakened Bones and Fractures
In most cases, bone tumors develop in the long bones of the upper arms and legs, and the pelvis. The tumors are usually benign but can be malignant. Cancer weakens the bone where the tumor exists and may cause fractures. Some individuals develop a noticeable limp or experience a sudden onset of severe pain in a bone that was previously sore, and this could be a sign of bone cancer. In some cases, x-rays for other conditions such as sprained ankles or knee injuries uncover benign tumors. Fractures in cancer-weakened bones can occur next to or through the bone tumor itself.

5. Low Back Pain
Bone cancer occurring in the pelvis may cause lower back pain and sciatica. Back pain is a widespread issue for adults, and this can delay a diagnosis of pelvic bone cancer. Individuals over the age of 45 are the demographic most commonly diagnosed with pelvic cancer, and diagnosis is often preceded by painful symptoms that last longer than a month. Affected people develop a sudden onset of back pain or sciatica that occurs primarily at night and becomes increasingly worse and unresponsive to changes in position or bed rest. Because there is no traumatic injury, most therapies to treat back pain are ineffective.

6. Fever
Most people with cancer contract a fever at some point. Although fever is rarely an early sign of bone cancer, it is a sign that the body is fighting an infection or illness. If cancer affects the immune system, it is harder for the body to fight off the infection. Fevers may signify that cancer has spread or is in an advanced stage. If pain accompanies the fever, or if it exceeds 103 F, seek medical attention.

7. Fatigue
Fatigue leaves people feeling exhausted after the simplest activities, and sleep does not improve the condition. Fatigue is an early symptom of most cancers, including bone cancer. Pain levels and anemia contribute to fatigue. However, medical professionals believe that anemia is directly related to the effects cancer has on the central nervous system, muscle-energy metabolism, and circadian rhythms. Poor nutrition can also contribute to fatigue in people with bone cancer.

8. Night Sweats
Some types of cancer cause night sweats, medically known as sleep hyperhidrosis. Overheating during sleep does not cause night sweats. Researchers believe the symptom has a connection with the hormonal changes that occur when diseases such as bone cancer affect the body. Night sweats could be the body's attempt to fight off cancer or a reaction to stress or anxiety. Fevers can also lead to sweating.

9. Loss of Appetite and Weight Loss
Another sign of bone cancer is the unintended loss of ten pounds or more. Weight changes and muscle loss are common cancer symptoms. Research shows that the body produces substances called cytokines, proteins created by both immune and non-immune cells, to fight off cancer. The production of cytokines causes a decrease in appetite, which leads to poor nutrition in addition to weight and muscle loss. Cachexia is a condition that causes extreme weight loss and muscle wasting, and is commonly seen in advanced cases of cancer.

10. Anemia
Bone cancer affecting the bone marrow may cause anemia, the lack of a healthy level of red blood cells or hemoglobin. Cancer interferes with the production of red blood cells, and low levels of hemoglobin prevent the body from getting the oxygen it needs. Symptoms of anemia include fatigue and weakness, shortness of breath, headaches, chest pains, irregular heartbeats, and lightheadedness. A physician can test for red blood cell levels using a complete blood count (CBC) test.

Tuesday, November 9, 2021
STOMACH CANCER,
Stomach cancer
Symptoms & causes
Diagnosis & treatment
Doctors & departments
Care at Mayo Clinic
Overview
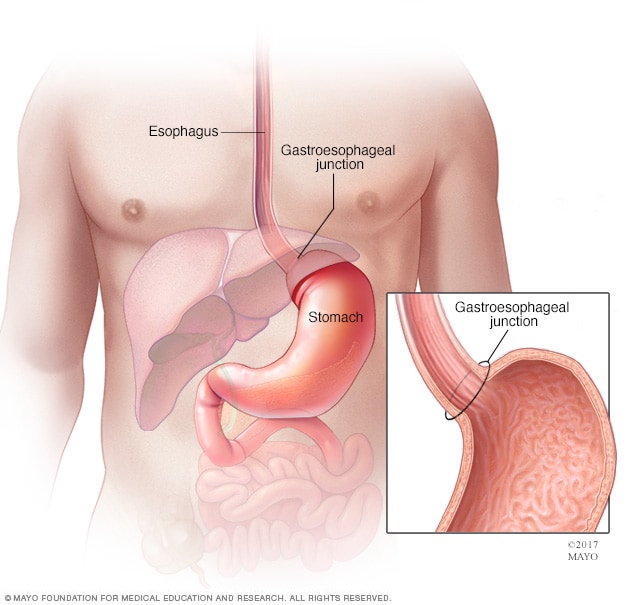
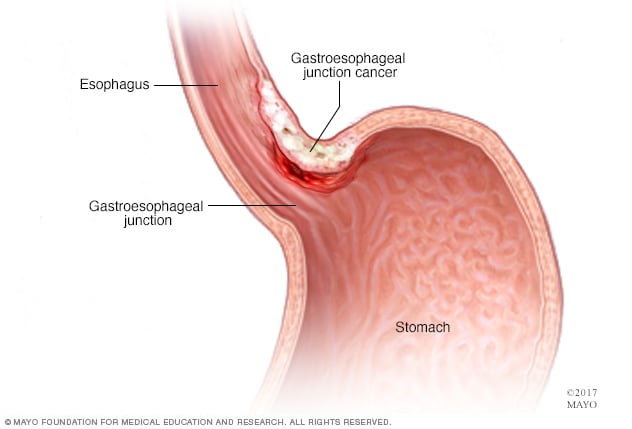
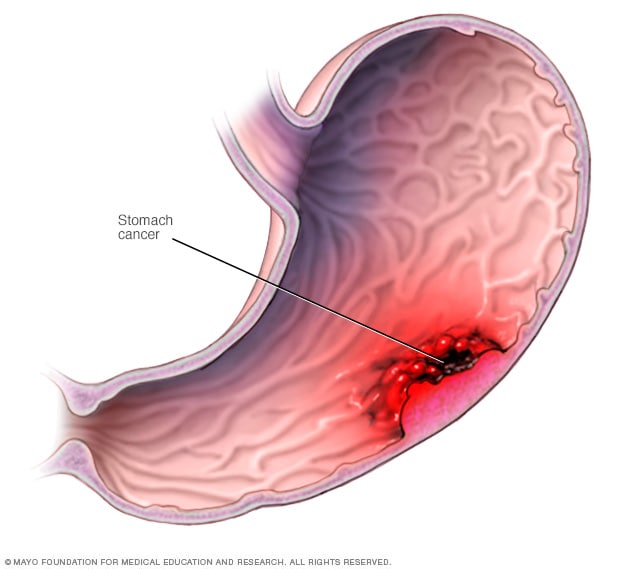
Stomach cancer is an abnormal growth of cells that begins in the stomach. The stomach is a muscular sac located in the upper middle of your abdomen, just below your ribs. Your stomach receives and holds the food you eat and then helps to break down and digest it.
Stomach cancer, also known as gastric cancer, can affect any part of the stomach. In most of the world, stomach cancers form in the main part of the stomach (stomach body).
But in the United States, stomach cancer is more likely to affect the area where the long tube (esophagus) that carries food you swallow meets the stomach. This area is called the gastroesophageal junction.
Where the cancer occurs in the stomach is one factor doctors consider when determining your treatment options. Treatment usually includes surgery to remove the stomach cancer. Other treatments may be recommended before and after surgery.
Products & Services
Book: Mayo Clinic Family Health Book, 5th EditionShow more products from Mayo Clinic
Symptoms
Signs and symptoms of stomach cancer may include:
Difficulty swallowing
Feeling bloated after eating
Feeling full after eating small amounts of food
Heartburn
Indigestion
Nausea
Stomach pain
Unintentional weight loss
Vomiting
When to see a doctor
If you have signs and symptoms that worry you, make an appointment with your doctor. Your doctor will likely investigate more-common causes of these signs and symptoms first.